September 20, 2022
Injury Management
Psychology
The role of psychology in tendinopathy treatment
Tendinopathy is a frequent pain in amateur and elite athletes. Its persistence can have a negative psychological impact and, consequently, a difficult rehab.
What is tendinopathy and what is its psychological impact on the patient?
Tendinopathy is often disabling, painful and persistent, and it describes a spectrum of changes in damaged tendons, which cause pain (related to the activity), and reduced function (due to mechanical load).
Even though there are many therapeutic modalities to treat tendinopathies, exercise and loading programs remain the most important and the most effective ones. However, in many cases, the disability could persist over 12 months, producing a negative psychological impact on patients (read reference 1,2 below).
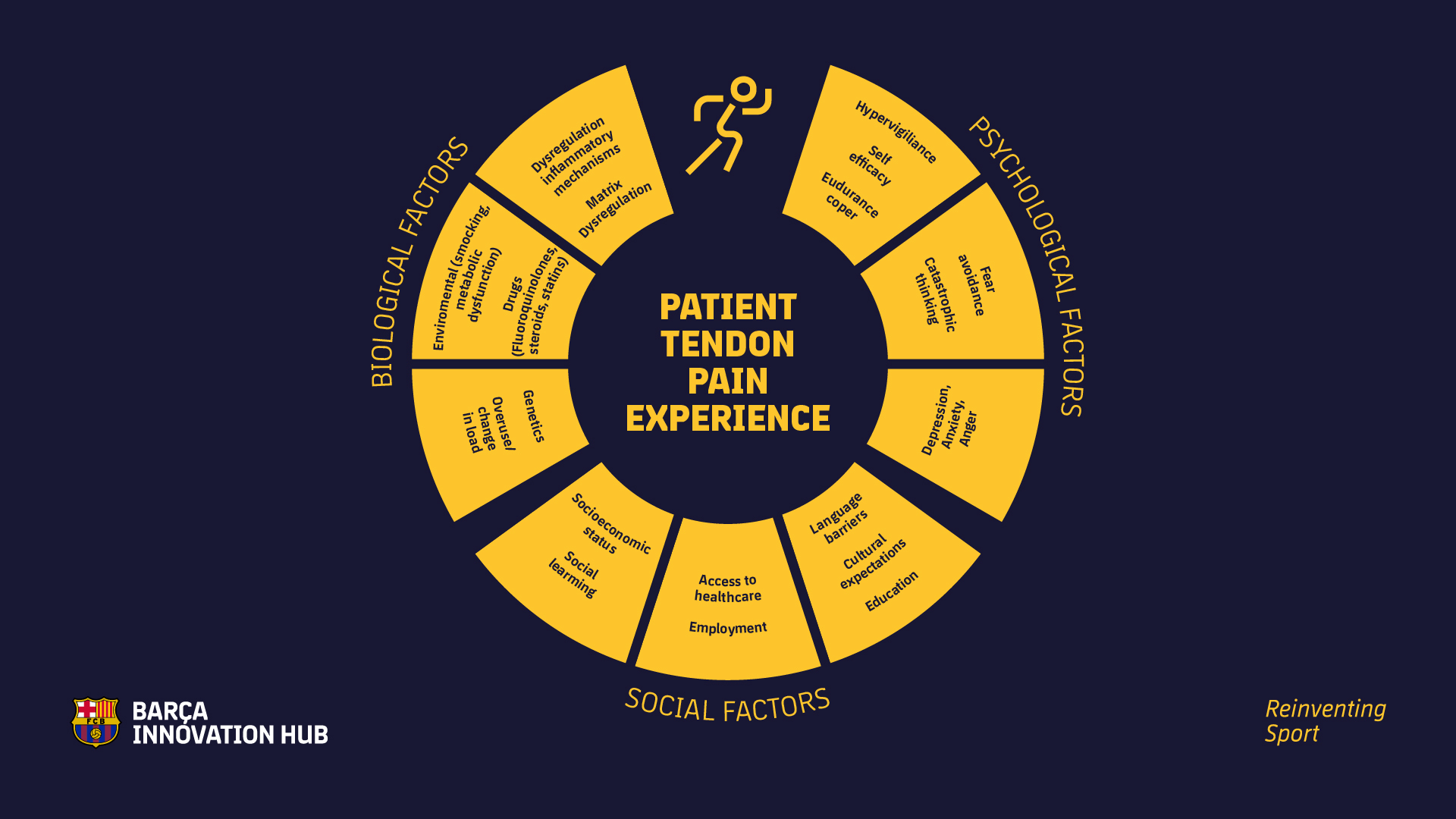
As it is explained in the study of Edgar N, Clifford C, O’Neill S, et al. Biopsychosocial approach to tendinopathy. BMJ Open Sport & Exercise Medicine (2022), on which this article is based, in most of the cases, the disabling effects of tendinopathies have a huge psychological impact which impedes optimal rehab. Luckily, there is increasing awareness of the influence that psychological and psychosocial components, such as self-efficacy and fear-avoidance, have in the outcomes of the rehab of musculoskeletal medicine (read ref. 3). For that reason, a proper approach to the different psychosocial factors could improve its prognosis and outcome.
Tendinopathy and elite athletes
In the case of elite athletes, especially in football, statistics and research show no particular problems with tendinopathies (even though Achilles’s tendinopathies are more frequent than patellar ones, for example). In any case, this information is uncertain since statistics usually only gather information about injuries when they prevent the footballer from playing games and/or from training.
However, in the case of professional footballers, it’s difficult to reach that point, since every injury or discomfort is monitored and assessed in very early stages, and it’s quickly put under control. What we can find, although epidemiologic studies don’t show it, are players that despite having a persistent pain don’t stop playing and don’t perform at their 100% either.
The case of amateur athletes is different: there is a significant number of cases with long-term advanced tendinopathy that, in many cases, forces the person to stop or to drastically reduce their activity.
Fear, anxiety and depression affect rehab
In chronic tendinopathies, it’s been proven that psychosocial factors such as fear, anxiety and depression affect pain and disability levels, which is detrimental for rehab. (read ref.4, 5). Under these chronic conditions, the individual’s perception of their ability to recover influences the relationship between pain and disability (read ref. 6–8). This is defined as self-efficacy: a high self-efficacy is related to lower pain and disability levels, and to a better physical functioning in general (read ref. 5).
Apart from self-efficacy, it has been proven that fear-avoidance also influences rehab outcomes. If the patient enters a cycle of pain avoidance and hypervigilance, disuse and avoidance of the physical activity could lead to kinesiophobia, beginning a harmful cycle of chronicity (read ref. 9, 10). Besides, this causes deconditioning of the musculoskeletal system,11 predisposing to further injury.
The medical team facing the patients’ psychology
According to the International Association for the Study of Pain (AISP), pain is influenced by biological, physiological, and social factors in variable degrees (read ref. 12). That’s why for the medical team is key to understand how those psychosocial factors could affect tendinopathy to educate patients about the possible influence they have on the pain experienced.
It’s also important to raise awareness in patients that not all the pain experienced is harmful, and that, in tendinopathy, the presence of pain is acceptable during rehab (read ref. 13). Self-efficacy may improve if individuals understand that the pain they experience is not likely to be causing further degeneration of the tendon. Taking all of this into account, it’s possible to reconsider the pain perception patients feel (read ref. 11).
However, for this approach to be effective, it’s necessary to have a close trustworthy relationship between the medical staff and the patients, to identify their barriers, and to understand the acceptable pain response of each of them (read ref. 14).
Patient empowerment
Patient education’s goal is to provide them with a greater understanding of the condition they are suffering (read ref. 15). In chronic conditions such as tendinopathy where loading programs are the initial treatment, educating patients is key to get optimal outcomes (read ref. 3). This element could be referred to as health literacy defined as patients having the ability to seek, and act on information relating to their health (read ref. 16, 17).
That is why the goal of successful patient education should always be patient empowerment, whereby the patient has the ability to largely self-manage their condition.
One of the main difficulties in loading programs to treat tendinopathy is that more than 50% of the patients abandon the treatment, which further perpetuates chronicity. Patients should understand how the program will benefit them, and it will be necessary to break the barriers that prevent adherence. In fact, it has been proven that patient empowerment in tendinopathy is key to facilitate adherence and commitment to the treatment (read ref. 18).
Biopsychosocial model and patient education
Biopsychosocial treatments recognise and approach biological, psychological, and social factors related to pain and disability. Nowadays, it is considered the most efficient treatment for chronic pain. Even though at present there isn’t solid evidence that analyses how psychosocial factors affect clinical outcomes in tendinopathies, findings in other musculoskeletal conditions help to reach the conclusion that reframing patients’ beliefs in pain and tendinopathy treatments will reduce the impact that psychosocial factors have on the rehab outcomes.
In this way, it is made evident that the biopsychosocial model that the patient could follow and learn will enable a faster rehab. In fact, a patient’s level of self-efficacy may be a stronger and reliable predictor of non-surgical outcomes than the structural defects that exist in imaging of different medical tests (read ref. 19, 20).
References:
-
Gillespie MA, M Cznik A, Wassinger CA, et al. Rotator cuff-related pain: patients’ understanding and experiences. Musculoskelet Sci Pract 2017;30:64–71.
-
Turner J, Malliaras P, Goulis J, et al. “It’s disappointing and it’s pretty frustrating, because it feels like it’s something that will never go away.” A qualitative study exploring individuals’ beliefs and experiences of Achilles tendinopathy. PLoS One 2020;15:e0233459.
-
Mallows A, Debenham J, Walker T, et al. Association of psychological variables and outcome in tendinopathy: a systematic review. Br J Sports Med 2017;51:743–8.
-
Woo AK. Depression and anxiety in pain. Rev Pain 2010;4:8–12.
-
Martinez-Calderon J, Zamora-Campos C, Navarro-Ledesma S, et al. The role of self-efficacy on the prognosis of chronic musculoskeletal pain: a systematic review. J Pain 2018;19:10–34.
-
te Wierike SCM, van der Sluis A, van den Akker-Scheek I, et al. Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sci Sports 2013;23:527–40.
-
Caneiro JP, Roos EM, Barton CJ, et al. It is time to move beyond ‘body region silos’ to manage musculoskeletal pain: five actions to change clinical practice. Br J Sports Med 2020;54:438–9.
-
Rondon-Ramos A, Martinez-Calderon J, Diaz-Cerrillo JL, et al. Pain neuroscience education plus usual care is more effective than usual care alone to improve self-efficacy beliefs in people with chronic musculoskeletal pain: a Non-Randomized controlled trial. J Clin Med 2020;9:2195.
-
Leeuw M, Goossens MEJB, Linton SJ, et al. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med 2007;30:77–94.
-
Kromer TO, Sieben JM, de Bie RA, et al. Influence of fear- avoidance beliefs on disability in patients with subacromial shoulder pain in primary care: a secondary analysis. Phys Ther 2014;94:1775–84.
-
Littlewood C, Malliaras P, Bateman M, et al. The central nervous system–an additional consideration in ‘rotator cuff tendinopathy’ and a potential basis for understanding response to loaded therapeutic exercise. Man Ther 2013;18:468–72.
- Raja SN, Carr DB, Cohen M, et al. The revised international association for the study of pain definition of pain: concepts, challenges, and compromises. Pain 2020;161:1976–82.
-
Malliaras P, Cook J, Purdam C, et al. Patellar tendinopathy: clinical diagnosis, load management, and advice for challenging case presentations. J Orthop Sports Phys Ther 2015;45:887–98.
-
Smith BE, Hendrick P, Bateman M, et al. Musculoskeletal pain and exercise-challenging existing paradigms and introducing new. J Sports Med 2019;53:907–12.
-
Fereidouni Z, Sabet Sarvestani R, Hariri G, et al. Moving into action: the master key to patient education. J Nurs Res 2019;27:1–8.
-
Nutbeam D. The evolving concept of health literacy. Soc Sci Med 2008;67:2072–8.
-
Paterick TE, Patel N, Tajik AJ, et al. Improving health outcomes through patient education and partnerships with patients. Proc 2017;30:112–3.
-
Sandford FM, Sanders TAB, Lewis JS. Exploring experiences, barriers, and enablers to home- and class-based exercise in rotator cuff tendinopathy: a qualitative study. J Hand Ther 2017;30:193–9.
-
Dunn WR, Schackman BR, Walsh C, et al. Variation in orthopaedic surgeons’ perceptions about the indications for rotator cuff surgery. J Bone Joint Surg Am 2005;87:1978–84.
-
Stubbs C, Mc Auliffe S, Mallows A, et al. The strength of association between psychological factors and clinical outcome in tendinopathy: a systematic review. PLoS One 2020;15:e0242568.
KNOW MORE
CATEGORY: MARKETING, COMMUNICATION AND MANAGEMENT
This model looks to the future with the requirements and demands of a new era of stadiums, directed toward improving and fulfilling the experiences of fans and spectators, remembering “feeling” and “passion” when designing their business model.
CATEGORY: FOOTBALL SPORTS PERFORMANCE
Through the use of computer vision we can identify some shortcomings in the body orientation of players in different game situations.
CATEGORY: MEDICINE HEALTH AND WELLNESS
A health check must detect situations which, despite not showing obvious symptoms, may endanger athletes subject to the highest demands.
CATEGORY: FOOTBALL TEAM SPORTS
In the words of Johan Cruyff, “Players, in reality, have the ball for 3 minutes, on average. So, the most important thing is: what do you do during those 87 minutes when you do not have the ball? That is what determines whether you’re a good player or not.”
CATEGORY: MEDICINE HEALTH AND WELLNESS SPORTS PERFORMANCE
Muscle injuries account for more than 30% of all injuries in sports like soccer. Their significance is therefore enormous in terms of training sessions and lost game time.
DO YOU WANT TO KNOW MORE?
- SUBSCRIBE
- CONTACT
- APPLY
KEEP UP TO DATE WITH OUR NEWS
Do you have any questions about Barça Universitas?
- Startup
- Research Center
- Corporate